19/08/2023 / Medical Advances
Epidemics: What Does the Future Hold?
Stay informed on the latest developing threats, cutting-edge technological innovations, and successful tactics for readiness in combating epidemic outbreaks.
Table of Content
The Impact of Globalization on Epidemics: A Look into the Future
Emerging Infectious Diseases: Predicting and Preparing for the Next Epidemic
Technology and Epidemic Control: Advancements and Challenges Ahead
Antimicrobial Resistance: A Looming Threat to Future Epidemics
The Intersection of Epidemics and Mental Health: Implications for the Future
Pandemic Preparedness and Response: Lessons Learned and Future Strategies
Vaccines and Immunization: Innovations and Controversies in Epidemic Prevention
The Future of Public Health: Building Resilient Systems to Combat Epidemics
Introduction
Prepare yourself for an enthralling delve into epidemic forecasting and preparation! In today's ever-changing society comprehending what could be ahead about epidemics becomes increasingly crucial. Come explore these topics with us:
Emerging infectious diseases - what potential risks lurk in upcoming years?
Climate change - how will it impact epidemics' spread, scale & intensity?
Technological advancements - what innovative tools could facilitate epidemic control and response
Public health strategies - how can we enhance our readiness and manage outbreaks better?
The Impact of Globalization on Epidemics: A Look into the Future
As we live in an interconnected society. Globalisation significantly influences epidemics. Understanding this complex relationship becomes crucial when considering how best to address these infectious diseases in the future. Here's' what to expect:
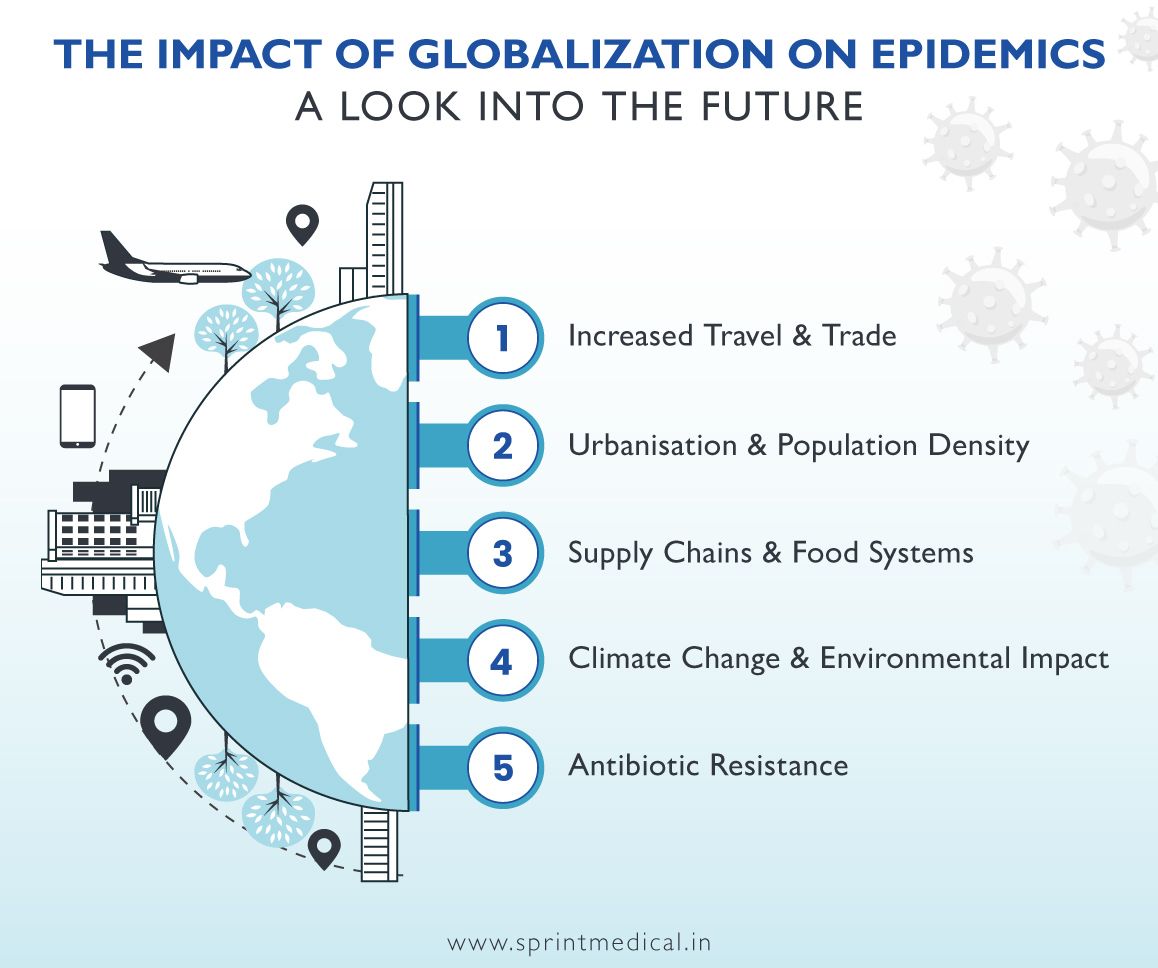
Increased Travel & Trade: Globalization plays a significant role in facilitating the rapid movement of people and goods; this expedited mobility results in infectious disease propagation across borders.
Urbanisation & Population Density: The formidable growth of urban areas accelerated by globalisation escalates crowding levels creating accommodating environments for pathogens that facilitate the transmission of diseases easily thus increasing morbidity rates globally.
Supply Chains & Food Systems: Complexity on Globalised supply chains quickly spread from contaminated goods into food systems spreading foodborne illnesses beyond national boundaries and leading to emergency health situations.
Climate Change & Environmental Impact: Globalisation links with climate change causing global response concerning ecosystem alterations which disrupt disease-carrying organisms' habitats hence geographic patterns changing these ecological transformations present greater disease risks worldwide
Antibiotic Resistance: Disseminating antimicrobial resistance through human conflict could threaten various sectors globally when microbes become resistant due to globalised activities. Issues such as resistant pathogens moving around under normal regulations lead to challenges faced by health institutions worldwide combating infectious diseases.
Emerging Infectious Diseases: Predicting and Preparing for the Next Epidemic
As we enter a new chapter of detecting infectious diseases, it’s important to remain cautious as we anticipate new strains to surface. Preparation towards preventive measures remains essential- especially so given the critical nature of public health today. Let us lend our focus on emerging infectious diseases through explorations on how best to predict, prevent, and help society respond effectively
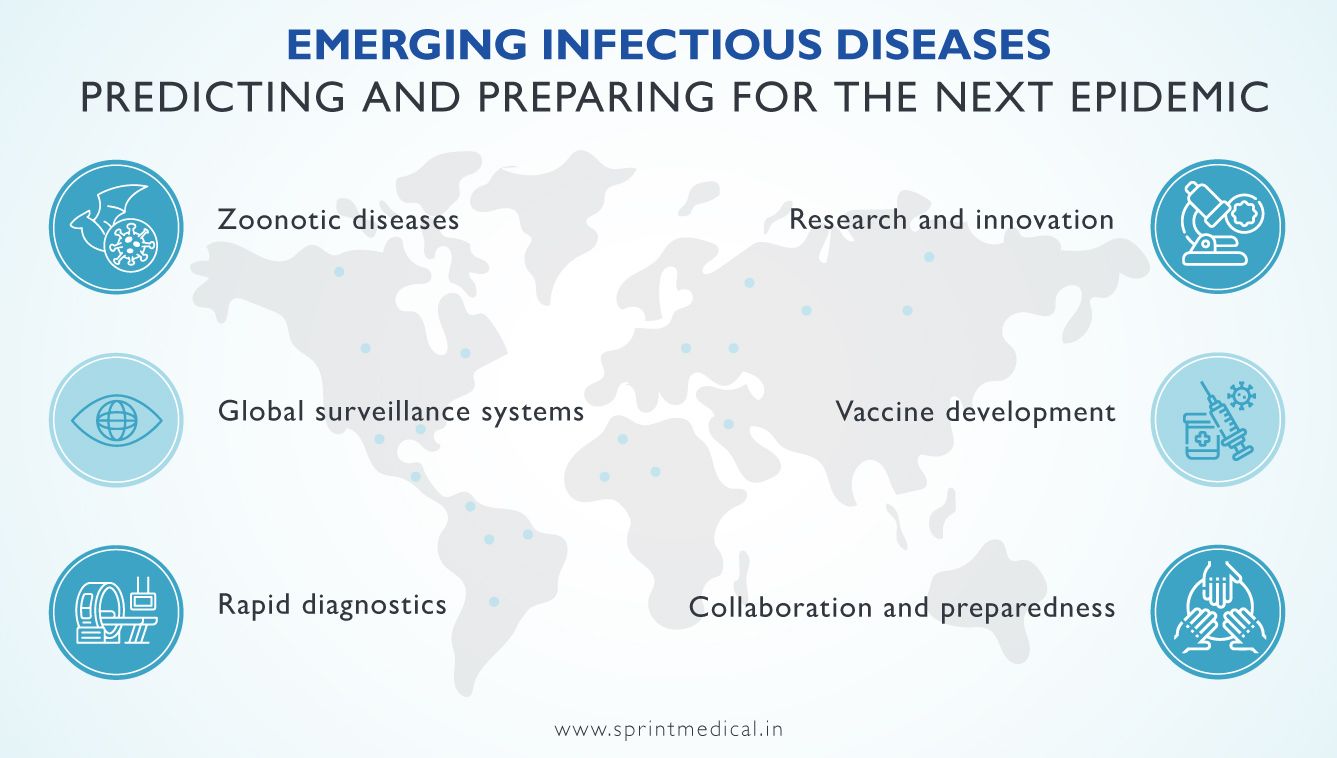
Zoonotic diseases: Many newly surfaced infections arise from animals called zoonotic diseases we need critically examine the reason behind how they crossed over from nature as an additional prevention tool
Global surveillance systems: Preventive measures require setting up global surveillance systems globally allowing early detection through careful monitoring patterns and trends of any future epidemics standing no chance when locating heavily infected sources inside local societies
Rapid diagnostics: Developing robust medical interventions with advanced diagnostic tools enables swift identification beyond timely treatment giving time for effective containment while reducing high-risk transmission rates significantly.
Research and innovation: Continuous innovation and research all form an integral part of understanding emerging infectious diseases with further studies focused on pathogen biology examining modes of transmissions with identifying possible interventions going forward
Vaccine development: Investing resources into vaccine development serves a pivotal role during outbreaks creating effective responses and limiting epidemic spread while providing cost-effective solutions to those in need.
Collaboration and preparedness: Global collaboration efforts thus increase during pandemics- effectively increasing partnerships between healthcare systems, policymakers along with researchers where wise preparation measures are put in place beforehand.
The Role of Climate Change in Shaping Future Epidemics
Due to its overall force on our world, it's no secret how climate change has influenced infectious diseases positively rising above the maximum survivable rate. Those who neglect the relationship between epidemics/climate will pay dearly for it as humankind progresses onward.
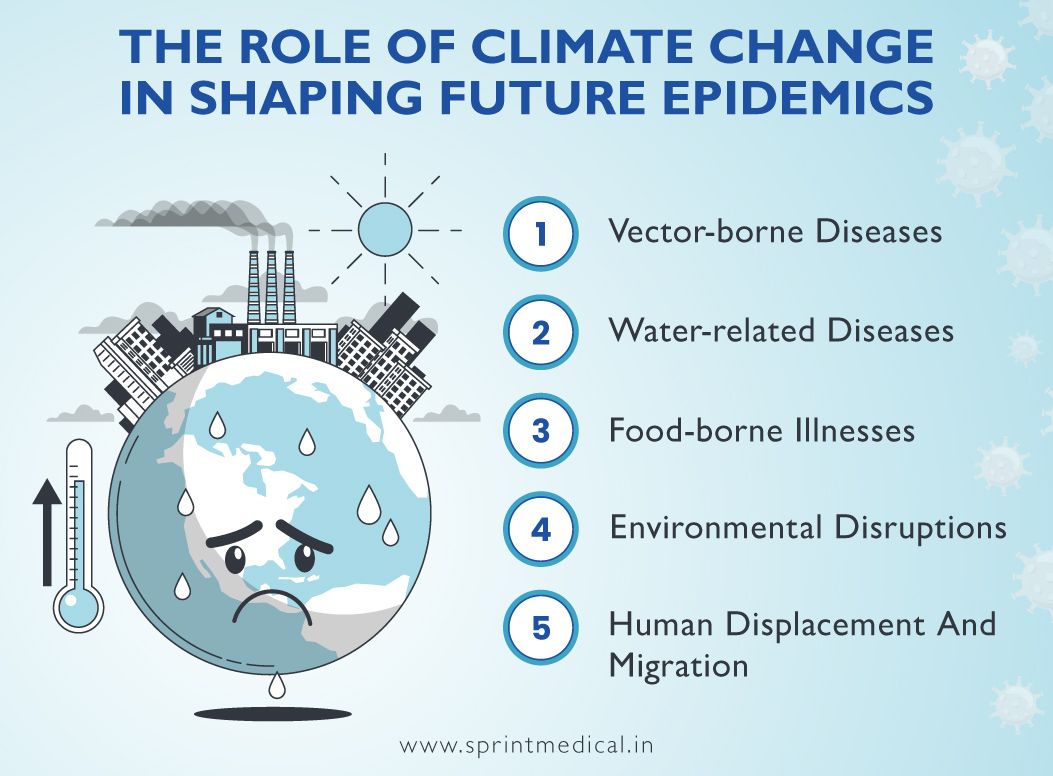
Exploring how this force manifests its impact on infectious diseases is vital:
Vector-borne Diseases: Major aspects like location, distribution, patterns, and behaviour of vectors aiding in disease transmission(Malaria, Ticks,)depend on a multitude of factors and climatic transformation. With temperature increases or precipitation changes, resultant modification could lead directly to increased illnesses such as Malaria Dengue Fever/Lyme disease prevalence,
Water-related Diseases: Rainfall patterns are part of changes climate change causes, which alter the quantity and availability of water. These transformations translate into natural disasters like Flooding, Drought worsening that affect water quality introducing easy proliferative conditions for water-borne illnesses-Cholera/Leptospirosis.
Food-borne Illnesses: Temperature and humidity can lead to changes in food production/storage, making increased levels of contamination higher, thus rising contamination levels causing high rates of foodborne illness, Listeriosis/Salmonella being good examples.
Environmental Disruptions: Climate change influences ecological balances affecting ecosystems' vulnerable as well as organisms in various ecosystems. All these alterations make it easy for a shift in the pathogen's geographical distribution. Along with susceptible populations, new environments, and new diseases can emerge, such as the Zika outbreak, becoming one serious concern.
Human Displacement And Migration: Rising sea levels/extreme weather events push people from their homes forcing them into extremely dangerous situations and creating specific outbreaks. However, such migrations also contribute to introducing infectious disease transmission risk in new areas.
Technology and Epidemic Control: Advancements and Challenges Ahead
In times when it's essential to combat epidemics head-on – technology acts as a vital tool offering innovative solutions for prevention, detecting and responding promptly. As we anticipate the challenges ahead, technological advancements continue presenting opportunities that require careful consideration.
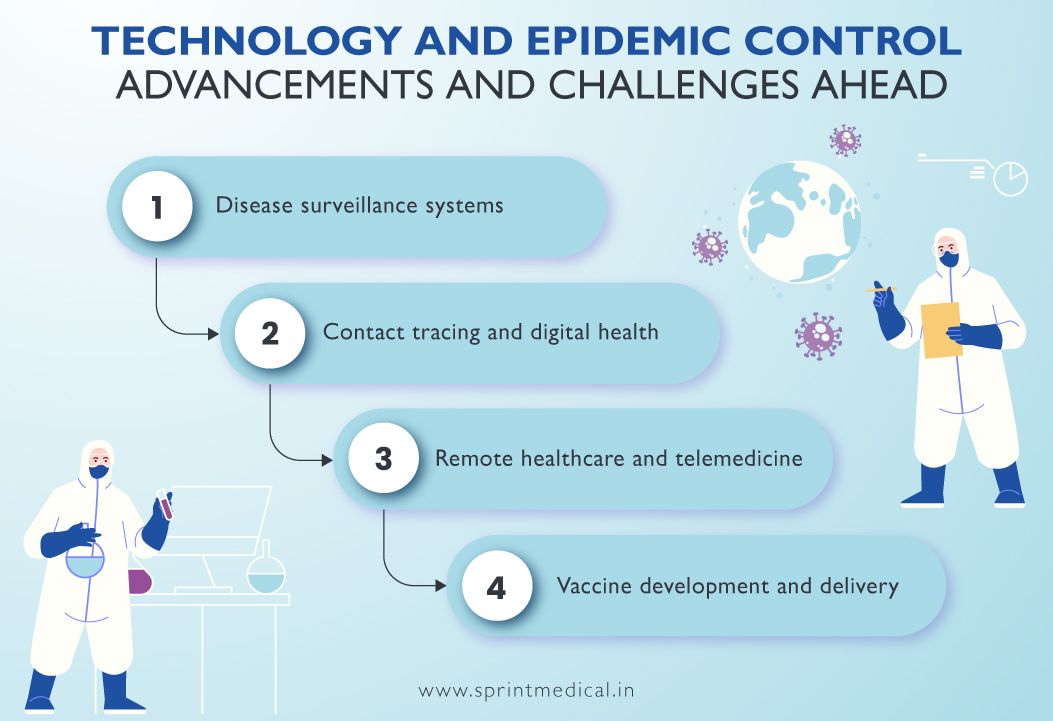
Disease surveillance systems: One significant area where technology offers a shield-aiding epidemic control is disease surveillance systems with real-time monitoring enabling early detection and rapid response during outbreaks of contagious diseases - digital platforms fueled by artificial intelligence or machine learning algorithms are prime examples of such capabilities these tools support.
Contact tracing and digital health: Contact tracing solutions supported by technological advances have helped limit exposure risks related to epidemics – aiding response efforts by positively identifying impacted individuals for recommendation on medically appropriate isolation measures expediently through mobile apps or wearable devices capable of providing precise location data more than ever before experienced
Remote healthcare and telemedicine: Prominent telemedicine services in response to pandemics are vital in ensuring that patients receive health care without physical contact within the healthcare setting. By providing virtual access to healthcare professionals, such services reduce the risks of transmission, thus minimising any interruptions during medical consultation appointments at this critical moment.
Vaccine development and delivery: Notably, mRNA-based vaccines represent impactful technological developments, enabling accelerated responses; logistical improvements ensure swift transport into remote locations through efficient cold chain monitoring systems that preserve vaccine efficacy throughout transit - significantly contributing towards containing epidemics.
Antimicrobial Resistance: A Looming Threat to Future Epidemics
Antimicrobial resistance (AMR) is a global concern of immediate urgency that has vast potential to significantly impact how we cure and prevent infectious diseases. As we peer into the future. The looming threat of AMR becomes increasingly evident. Let's explore why this challenge is critical and how it relates to possible future epidemics:
The emergence of drug-resistant pathogens: Antibiotic misuse or overuse has contributed greatly towards the emergence of antibiotic-resistant pathogens. Viruses, bacteria, and parasites have rendered existing treatments ineffective leading to difficulties in controlling their spread.
The challenge posed by limited treatment options: Growing intensity of antimicrobial resistance creates uncertainty about treatment options available for infectious diseases. This could make many previously manageable infections challenging to treat with catastrophic consequences for public health.
Increased need for expensive interventions and higher mortality rates: Antibiotic resistance leads to death rates increased compared to non-resistant strains in patients infected with resistant viruses, bacteria or parasites; managing drug-resistant infections often demands costlier interventions leading to further healthcare spending stress for already sapping systems.
Possible impact on controlling epidemics: The development of microbes resistant towards antibiotics can undermine efforts made towards containing an epidemic outbreak as no successful treatments are available; this increases their ability to spread more rapidly leading to larger outbreaks and raising stakes even more when dealing with potential or real public health pandemic.
The Intersection of Epidemics and Mental Health: Implications for the Future
Epidemics pose multiple risks- not only related to one’s physical well-being but also their mental state. Acknowledging this connection is crucial when envisioning future scenarios. In this article we'll explore the potential implications:
Psychological distress and anxiety: Fear of catching diseases like infectious pandemics can trigger feelings of intense psychological distress among individuals - social isolation and uncertainty further contribute towards anxiety levels.
Social and economic impact: Epidemics affect social structures and economies leading towards job loss, financial insecurity alongside social disconnection- these factors could result in the development of various Mental Health conditions.
Increased prevalence of mental disorders: Studies have indicated an alarming increase in depression rates along with post-traumatic stress disorders (PTSD) throughout pandemics; this condition is induced by experiences related to the outbreak.
Vulnerability of specific populations: Certain groups like health workers or those who already have underlying Mental Health conditions along with marginalised communities may require specific attention from policymakers so they may receive proper guidance or support.
Long-term consequences: Epidemics bring about challenges that have long-lasting effects on society such as chronic stress increasing suicide rates and an overburdened healthcare system- we must make more active attempts at addressing these issues now before they become more severe later on.
Pandemic Preparedness and Response: Lessons Learned and Future Strategies
The COVID-19 pandemic has been an urgent reminder of why we need to be fully prepared when dealing with global health crises. As we evaluate our lessons from this unprecedented situation, we must determine practical strategies geared towards delivering pandemic preparedness.
Strengthening healthcare systems: Strengthening healthcare systems is a key priority involving adequate investment infrastructure for medical facilities like hospitals coupled with investing in laboratory training, and workforce retention which will enable efficient testing combined with proper care delivery during any pandemic breakout.
Public health education and communication: Communicating sound public health education plans plays a significant role in combating unfounded myths alongside fostering public trust while promoting adherence to preventive measures too.
Educating the public about pandemics: including risks and appropriate preventive behaviour - is key to the early preparation required to deal appropriately when these issues arise going forward.
Research and development: Investment research & development fostering collaboration during diagnostics, and vaccine therapeutics facilitated during work produced provide much-needed ammunition in the fight against any pandemic breakout. Collaboration leads toward scientific progress leading to more effective interventions; useful tools are made available.
Anticipatory planning and scenario-based exercises: Scenario-based exercises coupled with anticipatory planning help identify gaps and refine response strategies effectively enhancing preparedness at all times. Evaluating and updating preparedness plans and regular moves towards readiness for future pandemics will ensure a proactive approach to tackling any crisis that may arise.
Vaccines and Immunization: Innovations and Controversies in Epidemic Prevention
Vaccines have had an enormous impact on epidemic prevention resulting in countless saved lives by reducing transmission rates of infectious diseases over time. Effective efforts placed on vaccine development research that bring success, particularly through improvements are notable milestones reached within this area of public health concern. However, it is crucial to also consider controversies that may surround the topics of vaccines and immunisation. Here we highlight key insights to further enlighten:
Vaccine development and efficacy: Over time, vaccines have been developed, paving the way for newer mRNA-based vaccines. Innovations in vaccine development continue to increase effectiveness levels and efficiency in countering epidemic spread.
Herd immunity and community protection: Vaccination not only provides individual protection but herd immunity as well when a substantial percentage is inoculated against the disease. It creates a protective barrier that prevents widespread transmission, safeguarding vulnerable individuals.
Vaccine hesitancy and misinformation: In some cases, controversies or lack of awareness generates hesitancy towards vaccination leading to misinformation dissemination. Proper education through open dialogue involving transparency on factual information is key to increasing awareness.
Safety and adverse events: Vaccination, like any medicinal intervention, involves risks where thorough testing screening is vital in detecting potential adverse effects early enough for timely resolution with rare occurrence cases bringing together improvements helping attain public trustworthiness among people discouraged by prior events after vaccination.
Equity in vaccine access: Access needs to be available to everyone as ensuring equitable access plays a significant role during epidemic prevention notwithstanding cost or location disparities as such barriers can be eliminated by proactive steps towards attaining global immunisation.
The Social and Economic Consequences of Future Epidemics
Epidemics are not isolated incidents; they affect society's multiple aspects beyond just healthcare services alone; acknowledging their potential consequences on social norms or economic fronts is essential while planning for the future proactively.
Here are some far-reaching implications of outbreaks:
Livelihood turmoil: Epidemics often lead to significant fluctuations in the economy resulting from extreme measures implementations like lockdowns that curtail everyday life activities & travelling besides imposing mandatory ‘social distancing. This unavoidably impacts businesses, resulting in job losses and straining individuals and recently bankrupted businesses’ financial capabilities.
Inequality & marginalisation exacerbation: Pre-existing inequalities are acknowledged to impact vulnerable populations such as minorities, marginalised groups, and low-income communities who suffer the most during epidemics. Unequal access to healthcare and adverse socio-economic outcomes create significant disparities that may take years to alleviate.
Education system disruption: School closures during outbreaks create significant challenges in the learning & development of the affected students. Taking education online further exacerbates the problem’s severity because disadvantaged students face a lack of online resources widening the learning gap even more so.
Healthcare infrastructure pressures: Epidemics can strain a country's healthcare systems tremendously - testing its very foundations especially if a pandemic expands erratically. This results in under-resourced healthcare services affecting non-COVID-related health concerns with potential delays or disruptions in such crisis times.
The Future of Public Health: Building Resilient Systems to Combat Epidemics
Preparedness through innovation and collaboration is key to mitigating future epidemics. Let us explore the crucial components of building resilient health systems:
Surveillance and early detection: Swift detection of disease outbreaks using advanced surveillance systems can greatly assist containment efforts while addressing the crisis on time.
Strengthening healthcare infrastructure: Investment into healthcare infrastructure that includes laboratories, medical supply chains, and facilities will be useful for concerted efforts during an epidemic situation
Capacity building and training: Building the workforce capacity by equipping healthcare professionals with training, and skill development opportunities ensure they have the relevant knowledge to handle complex situations associated with epidemics.
Research and development: As we continuously advance research particularly in areas like diagnostics or vaccines towards enhancing epidemic preparedness our progress strengthens us very positively
Global cooperation and coordination: International cooperation and collaborations enable sharing of resources that will yield a unified response creating better containment outcomes.
Community engagement and communication: Effective communication that involves trust-building measures including dissemination of accurate information is central to encouraging public participation during preventive measures.
Take-Home Points
Early detection and response are important for controlling epidemics.
Strengthening healthcare systems is also important to control epidemics effectively.
It's essential to promote proper education on clear communication techniques among healthcare facilities staff members on vaccine benefits to combat misinformation fueled by anti-vaccination movements effectively.
Research-based approaches could be used as evidence-based methods taking into consideration different demographic situations where particular societies may have different access options or opinions towards vaccines.
Antimicrobial resistance presents an often-underestimated challenge against mitigating disease transmission patterns across continents as pandemics often result from such transmissions facilitated by international travel patterns or weakened ecosystem changes.
Preparing for pandemics requires sustained investment beyond current circumstances in equipping public health systems with better equipment, and technologies while supporting continuous learning curricula to keep up with emerging trends and health threats.
References
FAQ on Epidemics: What Does the Future Hold?
Epidemic refers to the rapid spread of an infectious disease that potentially puts a specific population or geographical area at risk.
Localised outbreaks limited to specific areas define epidemics in comparison to pandemics which encompass extensive regions across countries or continents.
This contamination is historically traceable back to subjects ranging from human hygiene behaviour, increased international travel, and pathogen characteristics alongside population density levels.
Critical strategies that form part of epidemic prevention plans include public-awareness efforts, vaccination programs coupled with robust surveillance systems aimed at early detection capabilities and immediate response mechanisms upon outbreak alerts.
Vaccination strategies remain one of medicine's most effective methods for securing immunity against infectious diseases among populations. Immunity builds when vaccine administration prompts our immune system to create protective antibodies while introducing our immune system features towards detecting pathogens directly.
Public health officials have deployed advanced surveillance systems aimed at monitoring prevailing and emerging outbreaks. The process allows them to conduct timely interventions such as implementing isolation wards, and contact tracing efforts alongside public awareness campaigns.
Given globalisation's profound impact on travel networks, crowded urban settlement patterns, and trade interactions between potential epicentres at regional levels make cross-border transmission is more prevalent. International preparedness frameworks must emerge with robust global partnerships aimed more significantly than ever before towards containing epidemics/pandemics effectively.
Advanced technology plays a crucial role in epidemic control through contact tracing apps, telemedicine facilities, remote monitoring solutions, and rapid diagnostic tests among many others. Implementing advanced technology will assist with limiting exposure while containing and treating infectious diseases within a community.
One-way climate change can influence disease transmission and spread through alterations in temperature, precipitation patterns, and ecological settings - which have potential impacts on disease vectors or pathogens' distribution range.
Antimicrobial resistance occurs when pathogens such as bacteria or viruses no longer respond effectively to drugs used for treatment purposes. It presents substantive challenges towards regulating an epidemic spread while also increasing illness intensity.
Comments ( 0 )
No Comments
Leave a Comment
Health & Wellness Tips
Subscribe to our blog